What is an allergy?
An allergy is the response of the body’s immune system to normally harmless substances, such as pollens, foods, and house dust mite. Whilst in most people these substances (allergens) pose no problem, in allergic individuals their immune system identifies them as a ‘threat’ and produces an inappropriate response. This can be relatively minor, such as localised itching, but in more severe cases it cause anaphylaxis, a condition which can lead to upper respiratory obstruction and collapse and can be fatal.
 |
The most common causes of allergic reactions are:
1. Pollen from trees, grasses, and weeds (seasonal allergies or hay fever).
2. Dust mites.
3. Pet dander (from cats, dogs, or other animals).
4. Mold spores.
5. Insect stings and bites (e.g., from bees, wasps, or mosquitoes).
6. Certain foods (e.g., peanuts, tree nuts, eggs, milk, shellfish, wheat).
7. Medications (e.g., antibiotics, pain relievers, and some vaccines).
8. Latex.
9. Certain chemicals or substances.
10. Environmental factors (e.g., smoke, pollution, strong odors).
It is important to be aware of these common triggers and take appropriate precautions if you have known allergies to any of these substances. If you experience severe or life-threatening allergic reactions, seek immediate medical attention.
The most common causes of allergic reactions can vary depending on geographic location, individual sensitivities, and lifestyle. However, some allergens are more prevalent and widely recognized as common triggers for allergic responses. Here are some of the most common causes of allergic reactions:
1. Pollen:
Pollen from trees, grasses, and weeds is a common airborne allergen, leading to seasonal allergic rhinitis (hay fever) in many individuals.
2. Dust Mites:
These microscopic creatures are found in household dust, bedding, and upholstery, and their droppings can trigger allergic reactions, especially respiratory symptoms.
3. Pet Dander:
roteins found in the skin, fur, or saliva of cats, dogs, and other furry animals can cause allergies in susceptible individuals.
4. Mold Spores:
Mold grows in damp and humid environments and releases tiny spores into the air, which can be inhaled and cause allergic reactions, particularly in individuals with respiratory sensitivities.
5. Insect Stings:
Stings from bees, wasps, hornets, and fire ants can trigger localized or systemic allergic reactions, with the latter potentially leading to anaphylaxis.
6. Certain Foods:
Common food allergens include peanuts, tree nuts, soy, wheat, eggs, milk, fish, and shellfish. Food allergies can range from mild to severe and can affect both children and adults.
7. Medications:
Certain medications, such as penicillin and other antibiotics, can cause allergic reactions in some individuals.
8. Latex:
Latex allergy can be triggered by exposure to latex-containing products, such as gloves, balloons, and certain medical devices.
9. Inhalants:
Other airborne irritants, such as smoke, strong odors, and chemical fumes, can cause respiratory irritation in some people.
It's important to note that allergies can develop at any age, and individuals can be sensitive to multiple allergens simultaneously. Allergic reactions can manifest in various ways, ranging from mild symptoms like sneezing and itching to severe reactions like anaphylaxis, which requires immediate medical attention. If you suspect you have allergies or experience significant allergic reactions, consult a healthcare professional for proper evaluation, diagnosis, and management.
What happens when you have an allergic reaction?
When you have an allergic reaction, your body's immune system overreacts to a substance that is usually harmless to most people (an allergen). The immune system perceives the allergen as a threat and produces an inappropriate response, leading to a range of symptoms. The specific symptoms and their severity can vary depending on the type of allergen, the individual's sensitivity, and the route of exposure.
Here's what typically happens during an allergic reaction:
1. Exposure to Allergen:
You come into contact with an allergen, either through inhalation (e.g., pollen, pet dander), ingestion (e.g., food allergens), skin contact (e.g., latex, certain plants), or injection (e.g., insect stings).
2. Activation of the Immune System:
Your immune system recognizes the allergen as a threat, even though it is harmless to most people. In response, it produces specific antibodies, mainly immunoglobulin E (IgE), which are designed to fight the perceived threat.
3. Release of Chemicals:
Upon subsequent exposure to the allergen, the IgE antibodies trigger the release of various chemicals, including histamine, leukotrienes, and cytokines, from mast cells and basophils. These chemicals are responsible for the allergy symptoms.
4. Symptoms Manifest:
The release of chemicals leads to a wide range of allergic reaction symptoms, which can affect different parts of the body.
Common symptoms include:
- Respiratory symptoms: Sneezing, runny or stuffy nose, coughing, wheezing, and shortness of breath.
- Skin reactions: Hives (itchy, raised welts on the skin), eczema (inflamed and itchy skin), and contact dermatitis (skin rash upon contact with an allergen).
- Gastrointestinal symptoms: Nausea, vomiting, abdominal pain, and diarrhea, commonly triggered by food allergies.
- Anaphylaxis: In severe cases, a life-threatening systemic reaction can occur, affecting multiple body systems. Symptoms include difficulty breathing, swelling of the face and throat, a drop in blood pressure, and loss of consciousness.
5. Duration of Symptoms:
Allergic reactions can be immediate, occurring within minutes of exposure to the allergen (as in the case of anaphylaxis), or they can be delayed, taking several hours to manifest.
6. Treatment:
The treatment for allergic reactions depends on their severity. For mild to moderate symptoms, antihistamines or other over-the-counter medications may be sufficient. In more severe cases, especially for anaphylaxis, immediate medical attention is essential. Anaphylaxis requires the administration of epinephrine (adrenaline) through an auto-injector (e.g., EpiPen) and further medical management.
It's important to recognize and understand your specific allergens, avoid exposure whenever possible, and carry any necessary medications or emergency devices prescribed by your healthcare provider in case of severe reactions. If you suspect you have allergies or experience severe allergic reactions, seek medical evaluation and guidance to manage your condition effectively
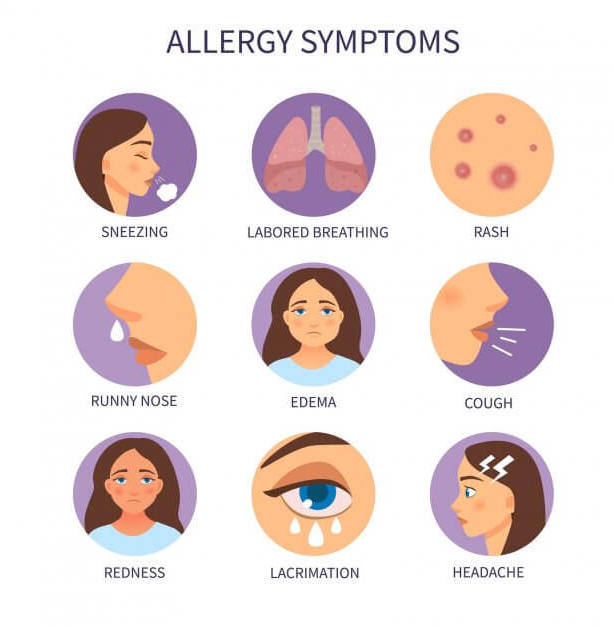
Symptoms of an allergic reaction include:
Common symptoms of an allergic reaction can vary depending on the type of allergen and the individual's sensitivity. The symptoms may affect different parts of the body and can range from mild to severe.
Here are some common symptoms of an allergic reaction:
1. Respiratory Symptoms:
- Sneezing
- Stuffy nose or runny (allergic rhinitis)
- Itchy or watery eyes (allergic conjunctivitis)
- Coughing
- Wheezing or shortness of breath
- Chest tightness or discomfort
2. Skin Reactions:
- Hives (red, raised, itchy welts on the skin)
- Eczema (inflamed, irritated, itchy skin)
- Contact dermatitis (skin rash upon contact with an allergen)
- Redness of the skin or Itching
3. Gastrointestinal Symptoms:
- Nausea
- Vomiting
- Abdominal pain or cramping
- Diarrhea
4. Anaphylaxis Symptoms:(A severe and potentially life-threatening allergic reaction)
- Difficulty breathing or wheezing
- Swelling of the face,tongue, or throat lips
- Rapid or weak pulse
- Drop in blood pressure
- Loss of consciousness or feeling faint.
5. Systemic Symptoms:
- Fatigue or weakness
- Headache
- Feeling lightheaded or dizzy
It's important to note that allergic reactions can vary from person to person, and some individuals may experience multiple symptoms simultaneously. The severity of the symptoms can also vary, with some people having mild reactions while others may experience severe allergic responses.
If you experience any symptoms of an allergic reaction, especially severe symptoms like difficulty breathing or signs of anaphylaxis, seek immediate medical attention. Allergic reactions can sometimes escalate rapidly, and prompt treatment is crucial for managing the situation effectively. If you have known allergies, it's essential to work with your healthcare provider to develop an action plan and identify triggers to minimize your risk of exposure to allergens.
Diagnosing an allergy?
Diagnosing an allergy typically involves a combination of medical history evaluation, physical examination, and allergy testing. The process is usually carried out by a healthcare professional, such as an allergist or immunologist.
Here are the common steps involved in diagnosing an allergy:
1. Medical History:
The healthcare provider will take a detailed medical history, including asking about your symptoms, their frequency and duration, and any potential triggers or patterns associated with the symptoms. They will also inquire about your personal and family history of allergies, asthma, and other related conditions.
2. Physical Examination:
The healthcare provider will perform a physical examination, focusing on any visible signs of allergic reactions or conditions.
3. Elimination Diet:
If the suspected allergen is related to food, the doctor may suggest an elimination diet. This involves temporarily removing suspected foods from your diet and then reintroducing them one by one to see if any trigger allergic reactions.
4. Allergy Testing:
- Skin Prick Test
- Blood Test (Specific IgE Test)
- Patch Test:
- Oral Food Challenge
5. Challenge Tests:
In some cases, a controlled challenge test may be conducted, where you are exposed to a suspected allergen under medical supervision to see if it triggers a reaction.
Once the diagnosis is confirmed, your healthcare provider will work with you to develop an appropriate management plan. This may involve allergen avoidance, medications (e.g., antihistamines, nasal corticosteroids), and, in some cases, allergen immunotherapy (allergy shots) to desensitize your immune system to specific allergens. The goal is to effectively manage your allergy symptoms and improve your quality of life.
Allergy testing
Allergy testing is a diagnostic procedure performed to identify specific allergens that trigger allergic reactions in an individual. The information obtained from allergy testing helps healthcare providers develop an appropriate management plan to reduce exposure to allergens and control allergy symptoms. There are several methods of allergy testing:
1. Skin Prick Test:
This is one of the most common and reliable allergy tests. During a skin prick test, a small amount of allergen extract (such as pollen, pet dander, food extracts) is placed on the skin, usually on the forearm or back. The skin is then lightly pricked or scratched through the drop of allergen. If you are allergic to the substance, a small raised bump (wheal) with surrounding redness (flare) will appear at the test site within 15-20 minutes.Skin Prick Test
2. Intradermal Test:
In some cases, an intradermal test may be performed, which involves injecting a small amount of allergen just beneath the skin surface. This test is more sensitive than the skin prick test but is typically reserved for specific situations where the skin prick test may not provide conclusive results.Intradermal Test
3.Blood Test (Specific IgE Test):
A blood sample is taken to measure the level of specific immunoglobulin E (IgE) antibodies produced by your immune system in response to specific allergens. This test is useful for individuals who cannot undergo skin testing due to skin conditions, extensive rashes, or the use of certain medications.Blood Test (Specific IgE Test)
4. Patch Test:
Patch testing is used to diagnose contact dermatitis (skin allergies) caused by exposure to certain substances, such as metals, fragrances, and preservatives. Small patches containing suspected allergens are applied to the skin and left in place for a specific period to see if a reaction occurs.Patch Test
5. Oral Food Challenge:
For suspected food allergies, a supervised oral food challenge may be conducted. During this test, you consume increasing amounts of the suspected food in a controlled setting to observe any allergic reactions.
It's important to note that allergy testing should be conducted by a qualified healthcare professional, such as an allergist or immunologist, in a controlled and safe environment. The results of allergy testing, along with your medical history and symptoms, will help determine the most effective approach to managing your allergies, which may involve allergen avoidance, medications, and allergen immunotherapy (allergy shots) if appropriate. Always consult with your healthcare provider to discuss the best testing options based on your specific situation.
How do I manage my allergy?
Managing your allergy involves a combination of strategies to reduce exposure to allergens and alleviate symptoms. Here are some key steps to manage your allergy effectively:
1. Identify and Avoid Triggers:
Determine the specific allergens that trigger your allergy and take steps to minimize your exposure to them. This may involve allergy testing to identify the specific substances you are allergic to. Once you know your triggers, you can take precautions to avoid them.
2. Maintain a Symptom Diary:
Keep a record of your allergy symptoms, including when and where they occur. This can help you identify patterns and potential triggers, making it easier to avoid them in the future.
3. Allergen Avoidance:
Take measures to minimize your exposure to allergens, such as:
- To alleviate the impact of high pollen seasons, it is advisable to keep windows closed.
- Using air purifiers with HEPA filters in your home to reduce airborne allergens.
- Regularly cleaning bedding, carpets, and curtains to reduce dust mites and pet dander.
- It is recommended to wear protective clothing while handling potential allergens.
4. Medications:
Use over-the-counter or prescription medications to manage allergy symptoms. These may include:
- Antihistamines: To alleviate sneezing, itching, and a runny nose.
- Decongestants:
To reduce nasal congestion.
- Nasal corticosteroids: To reduce inflammation and relieve nasal symptoms. - Eye drops: To provide relief for eyes experiencing itching and watering. - Topical creams or ointments: To manage skin allergy symptoms like itching and rashes.
5. Carry an Epinephrine Auto-Injector:
If you have a history of severe allergies or anaphylaxis, carry an epinephrine auto-injector prescribed by your doctor at all times. Ensure that both you and your close ones know how to use it.
6. Immunotherapy (Allergy Shots):
If your allergies are not well controlled with medications and allergen avoidance, your healthcare provider may recommend allergen immunotherapy. This involves receiving regular injections of small amounts of allergens over time to desensitize your immune system and reduce your sensitivity to those allergens.
7. Educate Yourself and Others:
Learn more about your allergy and its triggers. Educate your family, friends, and coworkers about your allergies and how they can help in case of an emergency.
8. Regular Checkups:
Schedule regular checkups with your healthcare provider to review your allergy management plan, adjust medications if necessary, and discuss any new or changing symptoms.
Remember, managing allergies requires a personalized approach. Work closely with your healthcare provider to develop a plan that suits your specific needs and lifestyle. By being proactive and consistent in your management, you can significantly improve your quality of life and reduce the impact of allergies on your daily activities.
The treatment of allergies typically involves a combination of preventive measures, lifestyle changes, and medical interventions. The specific approach depends on the type and severity of the allergy. Here are some common methods used in the treatment of allergies:
1. Avoidance of Allergens:
The first step in managing allergies is to identify and avoid the triggers whenever possible. This may involve staying indoors during high pollen seasons, using allergen-proof bedding and covers, and keeping pets out of specific areas.
2. Medications:
- Antihistamines:
These drugs block the action of histamine, a chemical released during an allergic reaction, and can help relieve itching, sneezing, and runny nose.
- Decongestants:
Used for nasal congestion, decongestants can help reduce swelling in the nasal passages.
- Nasal Corticosteroids:
These nasal sprays reduce inflammation in the nasal passages and are effective for allergic rhinitis.
- Eye Drops:
For allergic conjunctivitis, eye drops can alleviate itching and redness.
- Epinephrine: For severe, life-threatening allergic reactions (anaphylaxis), an epinephrine auto-injector (EpiPen) may be prescribed.
3. Immunotherapy (Allergy Shots):
Allergy shots, or immunotherapy, involve injecting small amounts of allergens into the body over time to desensitize the immune system. This treatment can be effective for those with severe allergies and can help reduce the need for long-term medication use.
4. Sublingual Immunotherapy (Allergy Tablets):
Instead of shots, sublingual immunotherapy involves placing allergen extracts under the tongue. It can be an alternative for certain allergies and is typically used for allergic rhinitis caused by pollen or dust mites.
5. Emergency Action Plan:
For individuals with severe allergies, especially those prone to anaphylaxis, having an emergency action plan is essential. This plan outlines steps to take in case of a severe allergic reaction and may include the use of an epinephrine auto-injector.
6. Lifestyle Changes:
Making lifestyle adjustments can also aid in managing allergies. Keeping the home clean and free of allergens, using air purifiers, washing hands frequently, and maintaining good hygiene can all be beneficial.
It's essential to work closely with a healthcare professional, typically an allergist or immunologist, to develop a personalized treatment plan based on the individual's specific allergies and medical history. A proper diagnosis and comprehensive management approach can significantly improve the quality of life for individuals with allergies.



















0 Comments