What is antibiotic resistance?
Antibiotic resistance is when bacteria develop the ability to survive exposure to antibiotics designed to kill them or stop their growth.
Antibiotic resistance is the ability of bacteria to resist the effects of antibiotics, a type of drug - such as penicillin or ciprofloxacin - that kills or stops the growth of bacteria. When bacteria become resistant to antibiotics, it makes it more difficult to treat diseases caused by those bacteria and limits the treatment options. Alternative treatments may be costly and, in some cases, toxic.
What are antibiotics?
Antibiotics are medicines that fight bacterial infections in people and animals. They work by killing the bacteria or by making it hard for the bacteria to grow and multiply.
Antibiotics can be taken in different ways:
Orally (by mouth). This could be pills, capsules, or liquids.
Topically. This might be a cream, spray, or ointment that you put on your skin. It could also be eye ointment, eye drops, or ear drops.
Through an injection or intravenously (IV). This is usually for more serious infections.
History of antibiotics
The history of antibiotics is a fascinating journey that began with the accidental discovery of penicillin and subsequently led to a revolution in medicine. Let's delve into the timeline of antibiotic development and the challenges posed by antibiotic resistance.
1928 - Discovery of Penicillin:
In 1928, Scottish bacteriologist Sir Alexander Fleming accidentally discovered penicillin while studying Staphylococcus bacteria. He noticed that a mold called Penicillium notatum inhibited the growth of the bacteria in a petri dish. This chance observation marked the beginning of the era of antibiotics.
1940s - Penicillin Production and WW II:
In the early 1940s, scientists Howard Florey and Ernst Chain successfully purified penicillin and demonstrated its effectiveness in treating bacterial infections. The mass production of penicillin during World War II saved countless lives and treated infections that were previously fatal. It was hailed as a "miracle drug."
1950s - Emergence of Resistance:
The widespread use of penicillin and other antibiotics led to the emergence of antibiotic-resistant strains of bacteria. By the 1950s, resistance to penicillin became a significant clinical problem. Bacteria with genetic mutations or the ability to transfer resistance genes became more prevalent.
1960s - Development of New Antibiotics:
Despite the challenge of resistance, the 1960s saw the development of new antibiotics like tetracycline, erythromycin, and methicillin. These drugs offered new hope in the fight against infectious diseases, but resistance to them also emerged over time.
1962 - Methicillin-Resistant Staphylococcus aureus (MRSA):
In 1962, the first case of methicillin-resistant Staphylococcus aureus (MRSA) was identified. MRSA was resistant to multiple antibiotics, making it difficult to treat and control infections.
1970s-2000s - More Antibiotics Introduced, But Resistance Persists:
Over the next few decades, numerous antibiotics from different classes were introduced to combat bacterial infections. However, the emergence and spread of resistance continued to be a challenge.
Recent Years - Slowing Antibiotic Development:
In recent years, the development of new antibiotics has slowed significantly. The discovery of new classes of antibiotics has become increasingly rare, partly due to the high cost and lengthy process of research and development.
Present Day - A Growing Threat:
Antibiotic resistance has become a global health threat, affecting both common and life-threatening infections. Resistant bacteria, often referred to as "superbugs," have the potential to cause widespread outbreaks and complicate medical treatment.
What causes antibiotic resistance?
The Challenge of Antibiotic Resistance:
The challenge of antibiotic resistance calls for a multifaceted approach. Efforts are underway to promote responsible antibiotic use, improve infection prevention and control measures, and invest in research to develop new antibiotics and alternative treatment options.
Antibiotic resistance is primarily caused by the overuse, misuse, and inappropriate use of antibiotics. Several factors contribute to the development and spread of antibiotic resistance:
1. Overuse of Antibiotics: The excessive use of antibiotics, both in healthcare settings and in agriculture, contributes to the development of resistance. When antibiotics are used more frequently than necessary, it provides more opportunities for bacteria to develop resistance.
2. Misuse of Antibiotics: Using antibiotics to treat viral infections, for which antibiotics are ineffective, is an example of misuse. Inappropriate prescribing or not completing the full course of antibiotics also contributes to the problem.
3. Inadequate Dosages: Administering antibiotics at suboptimal dosages can lead to incomplete eradication of bacteria, allowing resistant strains to survive and proliferate.
4. Antibiotics in Agriculture: The use of antibiotics in agriculture, particularly for growth promotion and disease prevention in livestock, can lead to the selection of resistant bacteria that can be transmitted to humans through food consumption.
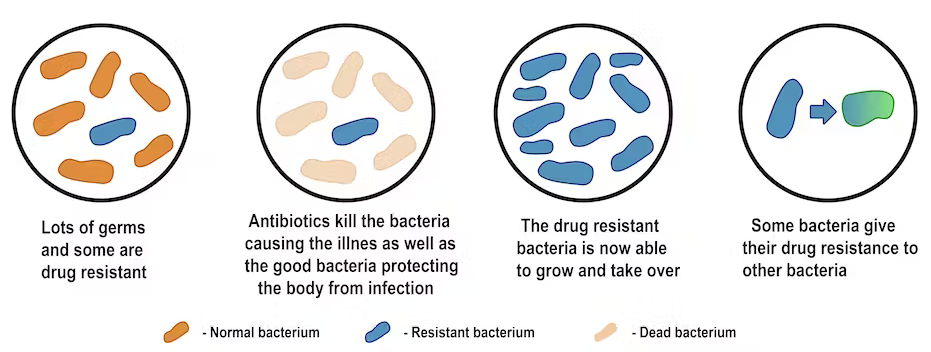
5. Transfer of Resistance Genes: Bacteria can acquire resistance genes from other bacteria through horizontal gene transfer, allowing the spread of resistance between different bacterial species.
6. Poor Infection Control: Inadequate infection prevention and control measures in healthcare settings can lead to the spread of resistant bacteria among patients.
7. Global Travel and Trade: The ease of global travel and trade facilitates the spread of resistant bacteria between countries and continents.
8. Lack of New Antibiotics: The development of new antibiotics has slowed in recent decades, limiting treatment options for resistant infections.
9. Environmental Contamination: The discharge of antibiotics into the environment, such as through sewage and waste from healthcare facilities, can contribute to the selection and spread of antibiotic-resistant bacteria in the ecosystem.
10. Lack of Public Awareness: Lack of awareness among the public and healthcare professionals about the consequences of antibiotic misuse and resistance can contribute to inappropriate antibiotic use.
11. Elderly and Immunocompromised Individuals: Certain vulnerable populations, such as the elderly and those with weakened immune systems, are more susceptible to infections, leading to higher antibiotic usage and increased selection pressure for resistance.
Addressing antibiotic resistance requires a concerted effort from healthcare professionals, policymakers, agricultural sectors, and the public. Implementing strategies to promote responsible antibiotic use, improve infection control practices, and invest in research for new antibiotics and alternative therapies is essential to combat the rise of antibiotic-resistant bacteria and protect the effectiveness of these essential medications.
Who is at risk for antibiotic resistance?
Antibiotic resistance can affect anyone, but certain individuals and populations are at higher risk due to specific factors. The following groups are particularly vulnerable to antibiotic resistance:
1. People Who Overuse Antibiotics: Individuals who frequently use antibiotics or misuse them by not completing the full prescribed course are at higher risk of developing antibiotic-resistant infections.
2. Patients in Healthcare Settings: People admitted to hospitals, long-term care facilities, or undergoing medical procedures are at increased risk of exposure to antibiotic-resistant bacteria. Healthcare-associated infections (HAIs) can be caused by drug-resistant organisms.
3. Immunocompromised Individuals: People with weakened immune systems, such as those undergoing chemotherapy, organ transplant recipients, or those with certain medical conditions, are more susceptible to infections, including drug-resistant ones.
4. Elderly Population: Older adults are more prone to infections and may have multiple health conditions requiring frequent antibiotic use, making them more susceptible to antibiotic-resistant pathogens.
5. People with Chronic Illnesses:Individuals with chronic health conditions, such as diabetes, heart disease, or respiratory disorders, may require repeated antibiotic treatments, increasing their risk of antibiotic resistance.
6. Children: Overuse or inappropriate use of antibiotics in children, especially for viral infections, can contribute to the development of antibiotic resistance.
7. Farm and Livestock Workers: Individuals working with animals in agriculture or livestock farming are at risk of exposure to drug-resistant bacteria through close contact with animals given antibiotics for growth promotion.
8. International Travelers: People who travel to regions with high rates of antibiotic resistance may acquire drug-resistant infections and bring them back to their home country.
9. Community Members: Antibiotic-resistant infections can also spread in the community through person-to-person contact, making the general population at risk.
10. Low-Income and Underserved Communities: Access to healthcare and appropriate antibiotics may be limited in some communities, leading to improper use of antibiotics and an increased risk of resistance.
11. Individuals with Recurrent Infections: People with recurrent infections may receive multiple courses of antibiotics, raising the risk of developing resistance.
Addressing antibiotic resistance requires efforts from both healthcare professionals and the public. Responsible antibiotic use, infection prevention and control measures, and raising awareness about the consequences of antibiotic misuse are essential to minimize the risk of antibiotic resistance and protect public health.
Mechanisms of antibiotic resistance
Antibiotic resistance can arise through various mechanisms that bacteria employ to evade the effects of antibiotics. These mechanisms enable bacteria to survive and proliferate in the presence of the drug. Some common mechanisms of antibiotic resistance include:
1. Enzymatic Inactivation: Bacteria produce enzymes that can modify or degrade the antibiotic molecules, rendering them ineffective. For example, beta-lactamase enzymes can break down beta-lactam antibiotics like penicillin and cephalosporins.
2. Altered Target Sites: Bacteria can alter the target sites of antibiotics, making them unable to bind effectively and inhibit bacterial growth. This alteration can occur through mutations in the target proteins or by reducing the number of binding sites.
3. Efflux Pumps: Bacteria may possess efflux pumps, which are specialized transport proteins that actively pump antibiotics out of the bacterial cell before they can exert their effects. This process reduces the intracellular concentration of the drug, leading to decreased efficacy.
4. Decreased Permeability: Some bacteria develop changes in their outer membrane or cell wall, reducing the entry of antibiotics into the bacterial cell and limiting their access to their target sites.
5. Biofilm Formation: Bacteria can form biofilms, which are protective communities of bacteria encased in a self-produced matrix. Within biofilms, bacteria are more resistant to antibiotics due to reduced drug penetration and altered metabolic states.
6. Acquisition of Resistance Genes: Bacteria can acquire genes responsible for antibiotic resistance through horizontal gene transfer. These resistance genes may come from other bacteria or from external sources like plasmids or transposons.
7. Hypermutation: Some bacterial strains undergo frequent mutations, leading to increased genetic variability. This process can accelerate the development of resistance to antibiotics.
8. Sporulation: Certain bacteria can enter a dormant, spore-forming state, which makes them less susceptible to the effects of antibiotics. Once conditions become favorable, the spores can reactivate and cause infections.
9. Collateral Sensitivity: In some cases, resistance to one antibiotic may result in increased sensitivity to another unrelated antibiotic, leading to selective pressure for the emergence of resistant strains.
These mechanisms can act individually or in combination, contributing to the complexity and diversity of antibiotic resistance in bacterial populations. The constant evolution of resistance poses a significant challenge in combating infectious diseases and underscores the importance of responsible antibiotic use, infection control practices, and the development of new antibiotics and alternative therapies.
Infections resistant to antimicrobial drugs
Antimicrobial drug resistance is indeed a significant global health concern. The emergence of infections resistant to commonly used drugs poses a serious threat to public health and healthcare systems. Here are some key points about infections resistant to antimicrobial drugs:
1. Bacterial Infections: Antibiotic-resistant bacterial infections are a major focus of concern. Diseases like pneumonia, tuberculosis, bloodstream infections (sepsis), and urinary tract infections are becoming harder to treat due to the rise of drug-resistant bacteria.
2. Gonorrhea: Gonorrhea, a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae, has developed resistance to multiple antibiotics, making it more difficult to treat and control.
3. Foodborne Diseases: Pathogens responsible for foodborne illnesses, such as Salmonella, Campylobacter, and E. coli, have also shown resistance to common antibiotics, raising concerns about food safety and proper infection control measures.
4. Tuberculosis: Drug-resistant strains of Mycobacterium tuberculosis, the bacterium responsible for tuberculosis (TB), have become a major challenge for TB control programs worldwide.
5. Viruses (e.g., HIV): Antiviral drug resistance is a concern, particularly in the case of viruses like HIV, where the virus can mutate and develop resistance to antiretroviral medications.
6. Parasites (e.g., Malaria): Malaria, caused by the parasite Plasmodium, has seen the emergence of resistance to several antimalarial drugs, posing obstacles to malaria control and elimination efforts.
7. Fungi (Candida auris): Fungal infections caused by Candida auris have shown multidrug resistance and are associated with high mortality rates, especially among hospitalized patients.
8. CDC's List of Drug-Resistant Threats: The Centers for Disease Control and Prevention (CDC) has identified 18 drug-resistant threats in the United States, classifying them into three categories: "urgent," "serious," and "concerning."
9. Monitoring and Prevention: Urgent and serious threats require intensified monitoring and prevention efforts to curb the spread of drug-resistant infections.
10. Ongoing Assessment: The CDC regularly re-evaluates and updates the list of drug-resistant threats as new challenges emerge in the field of antimicrobial resistance.
Addressing antimicrobial drug resistance requires a collaborative effort from healthcare professionals, policymakers, researchers, and the public. Implementing responsible antibiotic use, infection control measures, and investing in research and new treatment options are vital to combat this growing global health threat. Continued vigilance and coordinated action are necessary to preserve the effectiveness of existing antimicrobial drugs and develop strategies to tackle new drug-resistant infections effectively.
How antibiotic-resistant infections spread
Antibiotic-resistant infections can spread through various mechanisms, contributing to the global challenge of antibiotic resistance. Here are some common ways in which these infections can spread:
1. Person-to-person transmission: Resistant bacteria can be easily transmitted from person to person through direct contact, respiratory droplets, or contact with contaminated surfaces. This transmission can occur in hospitals, healthcare facilities, communities, and even within households.
2. Healthcare settings: Hospitals and healthcare facilities can serve as hotspots for the spread of antibiotic-resistant infections. Patients with compromised immune systems are more susceptible to acquiring such infections during medical procedures, surgeries, or prolonged hospital stays.
3. Food and water: Antibiotic-resistant bacteria can contaminate food and water sources. Consumption of contaminated food products, especially from animals treated with antibiotics, can lead to the transmission of resistant bacteria to humans.
4. Livestock and agriculture: The use of antibiotics in livestock and agriculture can contribute to the emergence and spread of antibiotic-resistant bacteria. Resistant strains can be transmitted to humans through the consumption of contaminated meat products or direct contact with animals.
5. Travel: International travel and migration can facilitate the global spread of antibiotic-resistant infections. Resistant bacteria can be carried by travelers and introduced to new regions, contributing to the dissemination of resistance.
6. Inadequate infection control: Poor infection control measures in healthcare settings and communities can facilitate the transmission of resistant bacteria. For instance, improper hand hygiene, inadequate sterilization of medical equipment, and suboptimal waste management can promote the spread of infections.
7. Overuse and misuse of antibiotics: Overuse and inappropriate use of antibiotics in both humans and animals are major contributors to antibiotic resistance. When antibiotics are unnecessarily prescribed or used incorrectly, they can promote the development of resistant bacteria.
8. Lack of new antibiotics: The dwindling pipeline of new antibiotics has led to limited treatment options for certain infections. This can lead to the increased use of existing antibiotics, potentially contributing to the selection and spread of resistant bacteria.
9. Horizontal gene transfer: Bacteria can acquire antibiotic resistance genes through horizontal gene transfer, where resistant genes are passed between different bacterial species. This genetic exchange can rapidly disseminate resistance across bacterial populations.
To combat the spread of antibiotic-resistant infections, it is crucial to implement comprehensive strategies that address appropriate antibiotic use, infection control measures, surveillance, and the development of new antibiotics. Additionally, public awareness and education about antibiotic resistance and responsible antibiotic use are essential to help mitigate the impact of this global health threat.
What are the symptoms of an antibiotic-resistant infection?
The Symptoms alone cannot definitively indicate whether an infection is caused by antibiotic-resistant bacteria. The signs and symptoms of infections caused by antibiotic-resistant bacteria are often similar to those caused by non-resistant bacteria, making it challenging for healthcare providers to distinguish between the two based solely on clinical presentation.
To identify antibiotic-resistant infections, laboratory tests are necessary. These tests involve obtaining samples from the infected area or site, such as blood, urine, sputum, or wound swabs, and culturing the bacteria to determine their susceptibility to various antibiotics. The process involves exposing the bacterial sample to different antibiotics to see which ones are effective in inhibiting or killing the bacteria. This helps determine which antibiotics will be most appropriate for treatment.
The testing process can take time, so doctors may prescribe broad-spectrum antibiotics initially to provide immediate treatment while waiting for the test results. Once the susceptibility profile is available, the healthcare provider can adjust the treatment to target the specific antibiotic-resistant bacteria.
It is essential for healthcare providers to be vigilant about the possibility of antibiotic-resistant infections, especially in individuals with risk factors, such as recent hospitalization, previous antibiotic use, or chronic health conditions. Taking a detailed medical history and conducting appropriate diagnostic tests are crucial steps in identifying and managing antibiotic-resistant infections effectively.
In summary, while symptoms can provide valuable clues about the presence of an infection, they cannot determine whether the infection is caused by antibiotic-resistant bacteria. Laboratory tests are necessary to confirm the type of bacteria involved and their susceptibility to antibiotics, enabling appropriate and effective treatment decisions.
How are antibiotic-resistant infections diagnosed?
The diagnosis of antibiotic-resistant infections involves a combination of clinical evaluation, medical history, and laboratory testing. Identifying antibiotic resistance in bacteria is crucial to ensure that the most effective treatment is administered. The diagnostic process generally includes the following steps:
1. Clinical Evaluation: The healthcare provider examines the patient's symptoms and conducts a physical examination to assess the signs of infection. They will also inquire about the patient's medical history, recent antibiotic use, hospitalizations, and exposure to healthcare settings.
2. Sample Collection: To identify the specific bacteria causing the infection and their susceptibility to antibiotics, samples are collected from the site of infection. Common samples include blood, urine, sputum, wound swabs, or other relevant body fluids.
3. Microbial Culturing: The collected samples are cultured in a laboratory setting. This involves placing the samples on specific media that encourage bacterial growth. The culture allows the bacteria to multiply, making it easier to identify and test them.
4. Identifying the Bacteria: Once the bacteria have grown in the culture, they are identified using various techniques, such as biochemical tests or molecular methods like Polymerase Chain Reaction (PCR). Identifying the specific bacteria is crucial for choosing appropriate antibiotics.
5. Antibiotic Susceptibility Testing: After identifying the bacteria, antibiotic susceptibility testing is performed. This test exposes the bacteria to different antibiotics to determine which ones effectively inhibit or kill the bacteria. The results provide a profile of the antibiotics that are effective against the specific bacterial strain.
6. Reporting Results: The laboratory provides a detailed report to the healthcare provider, indicating the bacterial identification and their susceptibility to different antibiotics. This report guides the choice of the most appropriate and effective antibiotic for treatment.
It's important to note that the process of culturing and testing bacterial samples can take time, usually ranging from 24 to 72 hours or longer, depending on the type of bacteria and the complexity of the tests. In some urgent cases, broad-spectrum antibiotics may be prescribed initially to begin treatment promptly, while waiting for the final susceptibility results.
Additionally, rapid diagnostic tests and technologies are being developed to streamline the identification of antibiotic-resistant bacteria and provide more targeted treatments. These advancements aim to improve patient outcomes and reduce the inappropriate use of antibiotics, which can contribute to the development of further resistance.
How are antibiotic-resistant infections treated?
The treatment of antibiotic-resistant infections can be challenging, as these infections are no longer susceptible to the usual first-line antibiotics. The choice of treatment depends on several factors, including the type of infection, the specific bacteria causing it, the severity of the infection, and the patient's medical history. Here are some general approaches and strategies for treating antibiotic-resistant infections:
1. Antibiotic Stewardship: Antibiotic stewardship programs aim to optimize the use of antibiotics to preserve their effectiveness. This involves using antibiotics judiciously, only when necessary, and for the appropriate duration. Overuse or misuse of antibiotics can contribute to the development of resistance.
2. Combination Therapy: In some cases, using a combination of antibiotics may be necessary to treat the infection effectively. This approach targets the bacteria from multiple angles, making it harder for them to develop resistance to all the drugs simultaneously.
3. Reserved or Last-Resort Antibiotics: Certain antibiotics are considered "reserved" or "last-resort" options and are only used when no other effective treatment is available. These antibiotics are often more potent and have a higher risk of adverse effects, so they are preserved for serious infections.
4. New Antibiotics: Pharmaceutical companies and researchers continue to develop new antibiotics to combat antibiotic-resistant infections. These novel drugs target different mechanisms to overcome bacterial resistance and expand treatment options.
5. Alternative Therapies: In some cases, alternative therapies like bacteriophages (viruses that target bacteria), monoclonal antibodies, or other immunotherapies may be considered for treatment. These therapies are still under investigation and may not be widely available.
6. Supportive Care: In severe infections, patients may require supportive care, such as intravenous fluids, respiratory support, and other measures to manage the symptoms and complications of the infection.
7. Infection Control Measures: In healthcare settings, strict infection control measures are essential to prevent the spread of antibiotic-resistant infections among patients and healthcare workers.
It's crucial for patients to follow their healthcare provider's instructions and complete the full course of antibiotics as prescribed, even if they start feeling better. Prematurely stopping the antibiotics can lead to treatment failure and increase the risk of resistance.
Prevention of antibiotic-resistant infections is equally important. Avoiding unnecessary antibiotic use, practicing good hand hygiene, and taking appropriate precautions in healthcare settings can help reduce the emergence and spread of antibiotic-resistant bacteria. Additionally, continued research and public health efforts are essential to address this global health challenge effectively.
Research on antibiotics resistance
Research on antibiotic resistance is a critical area of study due to its impact on public health and global healthcare systems. Scientists, researchers, and healthcare professionals are actively investigating various aspects of antibiotic resistance to understand its mechanisms, develop effective treatments, and implement strategies to combat its spread. Some key areas of research on antibiotic resistance include:
1. Mechanisms of Resistance: Researchers are studying the genetic and biochemical mechanisms behind antibiotic resistance in bacteria. Understanding how bacteria develop resistance helps in designing targeted interventions to prevent and combat it.
2. Novel Antibiotics: Scientists are exploring new classes of antibiotics or modifying existing ones to overcome resistance. The discovery and development of novel antibiotics are essential to expand the armamentarium against drug-resistant pathogens.
3. Antibiotic Stewardship: Research focuses on promoting responsible antibiotic use in healthcare settings and the community. Antibiotic stewardship programs aim to optimize antibiotic prescribing to reduce the development of resistance.
4. Combination Therapies: Investigating the use of combination therapies, where multiple antibiotics are used together, to combat drug-resistant infections is a growing area of research.
5. Phage Therapy: Phage therapy, using bacteriophages (viruses that infect and kill bacteria), is being explored as a potential alternative or complementary approach to antibiotics.
6. Alternative Treatments: Researchers are exploring non-antibiotic treatments, such as antimicrobial peptides, nanoparticles, and immune-based therapies, to combat infections caused by drug-resistant bacteria.
7. Surveillance and Tracking: Monitoring the prevalence and spread of antibiotic-resistant pathogens is crucial for public health interventions. Surveillance systems track resistance patterns globally.
8. Genomics and Bioinformatics: Advances in genomics and bioinformatics allow researchers to study the genetic makeup of bacteria, identify resistance genes, and trace their spread.
9. One Health Approach: Researchers are studying the interconnectedness of human, animal, and environmental health (One Health) to understand how antibiotic use in one sector impacts resistance in others.
10. Infection Prevention and Control: Research aims to improve infection control practices in healthcare settings to prevent the transmission of drug-resistant infections.
11. Public Awareness and Education: Studies focus on raising awareness and educating the public and healthcare providers about the responsible use of antibiotics and the consequences of antibiotic resistance.
12. Global Collaboration: International collaborations and partnerships between researchers, governments, and organizations are crucial in tackling antibiotic resistance, which knows no boundaries.
Research in these areas and others is essential to address the challenges posed by antibiotic resistance effectively. By developing innovative strategies, improving treatment options, and implementing evidence-based interventions, researchers aim to preserve the effectiveness of antibiotics and protect public health from the growing threat of drug-resistant infections.
What can I do to prevent antibiotic resistance?
Preventing antibiotic resistance is a collective effort that involves everyone, including individuals, healthcare providers, and policymakers. Here are some important steps you can take to help prevent antibiotic resistance:
1. Use Antibiotics Wisely: Only take antibiotics prescribed by a healthcare professional, and follow their instructions carefully. Do not share or use leftover antibiotics from previous prescriptions.
2. Complete the Full Course: Always complete the full course of antibiotics as prescribed, even if you start feeling better. Stopping antibiotics prematurely can lead to incomplete eradication of bacteria, increasing the risk of resistance.
3. Don't Demand Antibiotics Unnecessarily: Understand that antibiotics are not effective against viral infections like the common cold or flu. Avoid pressuring your healthcare provider for antibiotics if they are not necessary.
4. Practice Good Hand Hygiene: Regularly wash your hands with soap and water for at least 20 seconds, especially before eating, after using the restroom, and after coughing or sneezing. Hand hygiene is essential to prevent the spread of infections.
5. Vaccinate Yourself and Your Family: Stay up-to-date with vaccinations, as they can prevent many bacterial and viral infections, reducing the need for antibiotics.
6. Practice Safe Food Handling: Ensure proper food safety measures are followed to prevent foodborne infections. Cook food thoroughly, store it at the correct temperature, and avoid cross-contamination.
7. Limit the Use of Antibacterial Products: Antibacterial soaps and cleaning agents are not more effective than regular soap and water and may contribute to resistance. Use plain soap and water for handwashing and general cleaning.
8. Support Antibiotic Stewardship: In healthcare settings, support and participate in antibiotic stewardship programs that promote the appropriate use of antibiotics.
9. Prevent Infections: Take steps to prevent infections by maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep.
10. Educate Others: Spread awareness about antibiotic resistance and the importance of proper antibiotic use to friends, family, and your community.
Remember that preventing antibiotic resistance is a shared responsibility, and by adopting these practices, you can play a crucial role in preserving the effectiveness of antibiotics for future generations.










0 Comments