What is Parathyroid
gland?
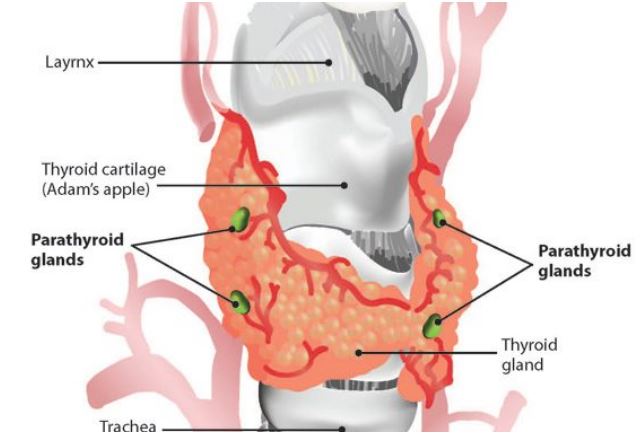
The parathyroid glands are small endocrine glands found in the neck
of humans and other tetrapods. Typically, humans have four parathyroid glands
that are located on the posterior surface of the thyroid gland, although their
specific positions can vary. These glands are responsible for producing and
secreting parathyroid hormone (PTH) in response to low blood calcium levels.
PTH plays a vital role in regulating the amount of calcium in the blood and
within the bones.
The parathyroid glands share a similar blood supply, venous
drainage, and lymphatic drainage with the thyroid glands. They originate from
the epithelial lining of the third and fourth pharyngeal pouches during
embryonic development. The superior glands arise from the fourth pouch, while
the inferior glands arise from the higher third pouch. The relative positions
of the inferior and superior glands can change due to the migration of
embryological tissues.
Hyperparathyroidism and hypoparathyroidism are conditions that
result from either excessive or deficient parathyroid function, respectively.
These conditions can lead to abnormalities in blood calcium levels and bone
metabolism.
Structure
The parathyroid glands are two pairs of glands located
behind the left and right lobes of the thyroid gland. Each gland has a flat,
lentil seed-like appearance with a yellowish-brown color. They typically
measure about 6 mm in length, 3 to 4 mm in width, and 1 to 2 mm in
anteroposterior dimension. Usually, there are four parathyroid glands in total.
The two upper glands on each side are known as the superior parathyroid glands,
while the lower two are referred to as the inferior parathyroid glands. In terms
of weight, healthy parathyroid glands weigh approximately 30 mg in men and 35
mg in women.
During a neck examination, the parathyroid glands are not
visible or palpable. They cannot be felt due to their small size and deep
location.
The drainage of the parathyroid veins occurs through the
superior, middle, and inferior thyroid veins. The superior and middle thyroid
veins ultimately drain into the internal jugular vein, while the inferior
thyroid vein drains into the brachiocephalic vein.
Lymphatic drainage
Lymphatic vessels
from the parathyroid glands have drainage into the deep cervical lymph nodes
and paratracheal lymph nodes.
In terms of
variation, the number of parathyroid glands can be variable. Typically, there
are three or more small glands located on the posterior surface of the thyroid
gland. However, some individuals may have six, eight, or even more parathyroid
glands. In rare cases, the parathyroid glands may be located within the thyroid
gland itself, in the chest, or even within the thymus. These variations
highlight the anatomical diversity that can exist in the positioning of the
parathyroid glands.
Microanatomy
The
parathyroid glands are distinct from the thyroid gland and serve a different
role in the body. They can be easily differentiated from the thyroid gland due
to their densely packed cells, which contrast with the follicular structure of
the thyroid gland.
Within
the parathyroid gland, two main types of cells can be found:
-
Chief cells: These cells are responsible for synthesizing and releasing
parathyroid hormone (PTH). They are small in size and appear dark when they are
loaded with PTH. When the hormone has been secreted or in their resting state,
they appear clear.
-
Oxyphil cells: These cells have a lighter appearance and their numbers tend to
increase with age. However, their specific function is not yet fully
understood.
The
presence of these distinct cell types within the parathyroid glands highlights
their unique role in hormone synthesis and secretion.
Function
The primary role of the parathyroid
glands is to maintain the balance of calcium and phosphate levels in the body
within a narrow range, crucial for proper functioning of the nervous and
muscular systems. This is accomplished through the secretion of parathyroid
hormone (PTH).
Parathyroid hormone, also known as
parathormone, is a small protein that plays a key role in the control of
calcium and phosphate homeostasis as well as bone physiology. It exhibits
antagonistic effects to those of calcitonin, another hormone involved in
calcium regulation.
When it comes to calcium regulation,
PTH increases the levels of calcium in the blood by directly stimulating
osteoblasts, which in turn indirectly stimulate osteoclasts through the
RANK/RANKL mechanism. This leads to the breakdown of bone tissue and the
release of calcium into the bloodstream. PTH also enhances gastrointestinal
absorption of calcium by activating vitamin D and promotes the reabsorption of
calcium by the kidneys, thus conserving it within the body.
In terms of phosphate regulation,
PTH acts as the primary regulator of serum phosphate concentrations by
influencing kidney function. It inhibits the reabsorption of phosphorus in the
proximal tubules of the kidneys. Additionally, PTH activates vitamin D, which
increases the absorption of phosphate in the intestines.
Overall, parathyroid hormone plays a
crucial role in maintaining the delicate balance of calcium and phosphate
levels in the body, ensuring optimal functioning of various physiological processes.
Disorders
Parathyroid disease is typically
classified into two main conditions based on the activity of the parathyroid
glands: hyperparathyroidism and hypoparathyroidism. These conditions are
characterized by specific symptoms resulting from either excessive or deficient
levels of parathyroid hormone in the bloodstream.
Hyperparathyroidism occurs when the
parathyroid glands become overactive and produce excessive amounts of
parathyroid hormone. This can lead to elevated levels of calcium in the blood
(hypercalcemia) and a decrease in phosphate levels. The symptoms of
hyperparathyroidism may include fatigue, weakness, bone pain, kidney stones,
frequent urination, abdominal pain, and digestive issues.
On the other hand,
hypoparathyroidism arises when the parathyroid glands are underactive or fail
to produce sufficient parathyroid hormone. This condition results in low levels
of calcium in the blood (hypocalcemia) and an increase in phosphate levels.
Symptoms of hypoparathyroidism may include muscle cramps, tingling or numbness
in the extremities, fatigue, anxiety, depression, dry skin, and hair loss.
The specific symptoms experienced by
individuals with parathyroid disease depend on the severity and duration of the
hormone imbalance, as well as individual factors. It's important to diagnose
and manage these conditions appropriately to restore the balance of parathyroid
hormone and maintain optimal calcium and phosphate levels in the body.
Hyperparathyroidism
Hyperparathyroidism is a condition
characterized by the excessive production of parathyroid hormone (PTH) by one
or more of the parathyroid glands. This leads to elevated levels of calcium in
the blood, a condition known as hypercalcemia. In the early stages of the
disease, individuals may not experience any noticeable symptoms.
When symptoms do occur, they can vary in severity and may include fatigue, weakness, bone pain or fractures, kidney stones, excessive thirst and urination, abdominal pain, constipation, nausea, loss of appetite, and mental confusion.
How does my body control parathyroid hormone levels?
That's correct. The secretion of
parathyroid hormone (PTH) is primarily regulated by a feedback mechanism
involving the levels of calcium in the blood. When blood calcium levels drop,
it triggers the release of PTH from the parathyroid glands. PTH then acts on
various target organs to increase calcium levels in the blood.
Conversely, when blood calcium
levels rise, it inhibits the release of PTH, preventing further elevation of
calcium. This feedback loop helps maintain calcium homeostasis in the body.
However, certain conditions can
disrupt this feedback loop and cause abnormalities in PTH secretion. For
example:
1. Primary Hyperparathyroidism: This
occurs when one or more parathyroid glands become overactive and produce
excessive amounts of PTH, leading to high blood calcium levels. It is most
commonly caused by a benign tumor, known as a parathyroid adenoma.
2. Secondary Hyperparathyroidism: In
this condition, the parathyroid glands react to low blood calcium levels caused
by other factors, such as chronic kidney disease or vitamin D deficiency. As a
result, the glands release excess PTH to compensate for the calcium imbalance.
3. Hypoparathyroidism: This
condition occurs when the parathyroid glands are unable to produce sufficient
amounts of PTH. It can be caused by damage to the parathyroid glands during
surgery or autoimmune conditions that affect their function. Hypoparathyroidism
leads to low blood calcium levels and sometimes high phosphate levels.
What test checks parathyroid hormone levels?
Yes, that's correct. The levels of
parathyroid hormone (PTH) can be assessed through a blood test. Here's how the
process typically works:
1. Blood Sample Collection: A healthcare
provider will use a needle to draw a blood sample from a vein in your arm. They
will clean the area with an antiseptic, apply a tourniquet to make the veins
more prominent, and insert the needle to collect the blood into a tube.
2. Laboratory Testing: The blood
sample is then sent to a laboratory for analysis. In the laboratory, the sample
is processed, and the PTH levels are measured using specialized tests.
3. Evaluation of Results: The
laboratory will provide the results of the PTH test, indicating the specific
level of parathyroid hormone in your blood. The results are typically reported
in picograms per milliliter (pg/mL) or picomoles per liter (pmol/L).
4. Interpretation and Consultation:
Your healthcare provider will review the test results and interpret them in the
context of your overall health and medical history. They will discuss the
findings with you and explain what the results mean in terms of your
parathyroid function.
What are normal parathyroid hormone levels?
That's correct. The normal range for
parathyroid hormone (PTH) levels can vary slightly between different
laboratories. It's important to refer to the specific reference range provided
by the laboratory that conducted your blood test. However, as a general
guideline, the normal range for the "PTH, intact" blood test is
typically reported as 15 to 65 picograms per milliliter (pg/mL).
It's essential to interpret the test results in the context of your overall health and medical history. Your healthcare provider will review your results, taking into consideration factors such as your symptoms, medical conditions, and other laboratory findings, to determine the appropriate course of action. If your PTH levels fall outside the normal range or if there are other indications of parathyroid dysfunction, your healthcare provider may recommend further testing or consultation with an endocrinologist, a specialist in hormonal disorders.
Remember, individual circumstances
may vary, and it's crucial to follow the guidance of your healthcare provider
regarding the interpretation and management of your PTH levels.
What happens if parathyroid hormone levels are high?
That's correct. When there are high
levels of parathyroid hormone (PTH) in the blood, it can lead to an excess of
calcium (hypercalcemia) and a decrease in phosphorus levels (hypophosphatemia).
This occurs because PTH helps regulate calcium and phosphorus balance in the
body.
High levels of calcium in the blood
can cause symptoms such as:
1. Fatigue and weakness
2. Excessive thirst and frequent
urination
3. Digestive issues like nausea,
vomiting, and constipation
4. Bone pain or joint pain
5. Kidney stones
6. Abdominal pain
On the other hand, low levels of
phosphorus in the blood can cause symptoms such as:
1. Weakness and muscle pain
2. Loss of appetite
3. Bone and joint pain
4. Fatigue and difficulty
concentrating
5. Respiratory problems
6. Changes in mood or behavior
It's important to note that these
symptoms can vary in severity depending on the individual and the extent of the
calcium and phosphorus imbalance. If you are experiencing any of these symptoms
or if you have concerns about your parathyroid hormone levels, it's best to
consult with your healthcare provider for a proper evaluation and further
guidance.











0 Comments